Spasticity Management
Spasticity (a.k.a. hypertonicity) is an abnormal increase in muscle tone or stiffness of muscle which may cause problems with movement, pain, spasms, hygiene, deformity, function and independence. It is usually caused by damage to nerve pathways within the brain or spinal cord that control muscle movement. It is estimated that it affects between 17-39% of stroke, >90% of cerebral palsy, 60-80% of multiple sclerosis, and 65-67% of spinal cord injury patients.
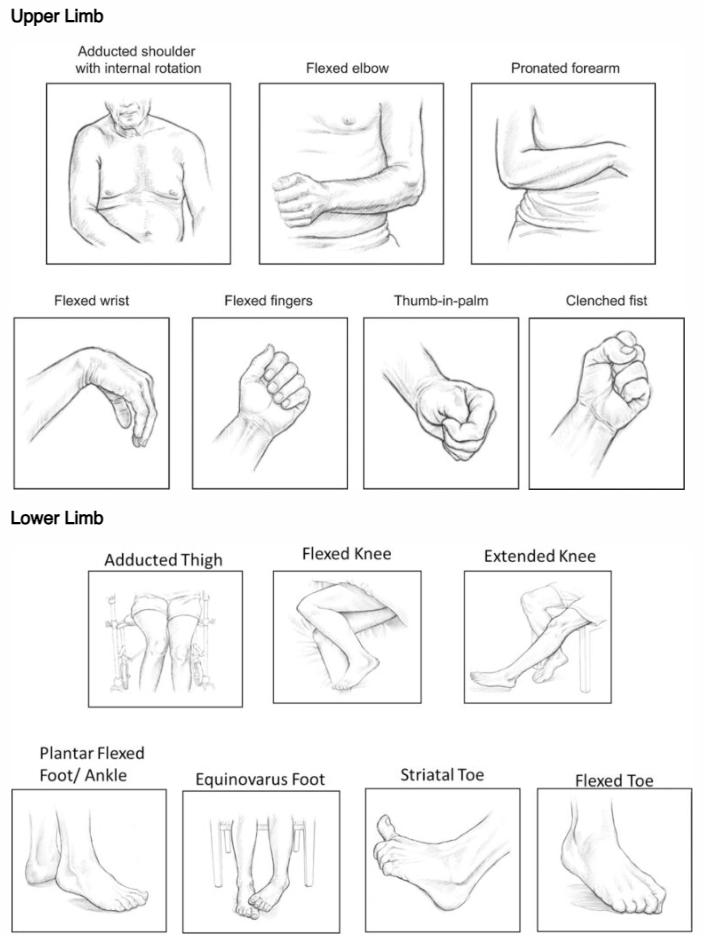
SYMPTOMS
Symptoms commonly associated with spasticity include hypertonicity (increased muscle tone), clonus (a series of rapid muscle contractions), exaggerated deep tendon reflexes, painful muscle spasms, and fixed joints (contractures).
MANAGEMENT
Patient and carer education
- Daily stretching and range of motion (ROM) exercises
- Avoidance of noxious stimuli (e.g., infections, pain, pressure ulcers, urinary retention, ingrown toenails)
- Proper positioning, daily skin inspection, adequate bladder/bowel programs
Physical therapy
- Repeated, gradual, sustained stretching
- Orthoses (splints)
- Serial casting (progressive application of fibreglass cast)
- Can be combined with Botulinum toxin injections
- Best results are achieved by working with a specialist Physiotherapist, Occupational Therapist (OT), or Exercise Physiologist (EP)
Medications:
- Oral medications such as baclofen, dantrolene, diazepam, or clonazepam.
- Used for generalised spasticity
- Use is limited by side effects such as drowsiness and hepatic impairment
Nerve/Motor Point Blocks:
- Botulinum toxin injections
- Phenol neurolysis
Surgery
- Considered for severe spasticity following failure of pharmacological/non-pharmacological measures
- Tendon lengthening
- Tendon Transfers
- Intrathecal Baclofen pump insertion
- Microsurgical Dorsal Root Entry Zone (DREZ)
- Peripheral neurotomy
BOTULINUM TOXIN INJECTIONS
Botulinum toxin type A (BoNT-A) is the most widely used neurotoxin to treat spasticity. It causes temporary, focal muscle weakness by blocking the release of acetylcholine at the neuromuscular junction. It is administered as an intramuscular injection guided by ultrasound, electromyography, nerve stimulation or a combination of these to correctly identify the muscle. The effect may last up to 3 months, with nerve sprouting and re-innervation leading to functional recovery of the muscle. Therefore, injections need to be repeated.
It is a safe intervention for spasticity however, there may be adverse effects including allergic responses, generalised weakness, or flu-like symptoms. Multiple injections of BoNT-A may lead to the production of neutralising antibodies which exacerbate an immune response and lead to treatment failure in some patients. However, this is minimised with newer preparations of the drug.
Focal BoNT-A injections may be used to reduce overactivity in specific muscle groups in order to improve selective movement control. It may also enable stretching and lengthening of muscles to prevent the progression of contractures and thus provide a window of opportunity to maximise gains during physical rehabilitation.
GOALS OF TREATMENT
- Improve independence
- Improve limb position and function
- Improve mobility
- Improve hygiene
- Reduce falls risk
- Reduce pain
- Reduce analgesic requirements
- Reduce the burden of care
- Reduce or prevent spasms
- Prevent contractures and avoid surgery







